WHAT YOU NEED TO KNOW ABOUT CONCUSSIONS AND INSURANCE LAW
- October 20, 2021
- admin
- No comments

By Cary N. Schneider, Partner, Schneider Law Firm
August 1, 2019
Introduction
A concussion is the most common type of mild traumatic brain injury and often has serious consequences that are frequently not managed properly. Unfortunately, concussions are hard to diagnose, difficult to appreciate, and not well understood. Make no mistake about it, the consequences of misdiagnosis or faulty management that can lead to major disability or death. It is important to appreciate that the law does recognize the seriousness of a concussion and the impact on a claimant’s entitlement to compensation. In the accident benefits world, a properly diagnosed concussion takes a claimant outside of the minor injury guidelines. In the tort regime, the existence of post-concussive symptoms have been influential in finding that a claimant has suffered a threshold injury and entitlement to damages. It is important for lawyers, adjusters, treating medical practitioners, adjudicators, and judges to have an understanding of the medicine and the law when dealing with an allegation of a mild traumatic brain injury.
The Mechanism Of A Concussion
The exact mechanism of a concussion is unknown. Axon tearing occurs in more severe brain injuries, but proof is lacking for this mechanism in concussion. It is more likely that concussion is due to rotational acceleration of the brain (jiggling of the brain) that produces a disordered metabolic cascade or biochemical injury such as altered metabolism of glucose or derangement of adenine nucleotides. In most people, symptoms occur within the first seven to ten days and resolve within three months. Sometimes, post-concussive symptoms may persist on an ongoing basis and lead to significant adverse consequences.[1]
Second-impact syndrome occurs when a concussed person, (especially a younger person), returns to engaging in physical activities before complete recovery and sustains a second brain injury. Also, repeated concussions may cause delayed post-traumatic brain degeneration, leading to dementia and movement disorders similar to Alzheimer and Parkinson diseases.[2]
It is now well understood in the medical literature that direct impact to the head is not required to have suffered a concussion. For example, concussions can occur with a blow to the chest; which may cause a whiplash effect on the brain. Whiplash of the neck and concussions frequently co-exist. In addition, the loss of consciousness is not a requirement for a concussion and in fact only has occurred in 5% of known cases. [3] It is inaccurate and dangerous to rule out a diagnosis of a concussion simply on the basis that an individual was not knocked unconscious.
The young brain is more susceptible to concussion than the adult brain and may require more time to recover. After suffering one concussion, there is greater susceptibility to sustaining further concussions. In addition, subsequent concussions often occur with less force and take longer to resolve. The statistics show that females are more susceptible to concussions than males, and that there may be a genetic factor underlying susceptibility to concussion.[4]
The Challenge Of Diagnosing A Concussion
The diagnosis of concussion is not easy and requires a knowledgeable physician and a cooperative patient. In the absence of both, accurate diagnosis and management may not be possible. For instance, a concussed athlete may minimize the symptoms in order to not miss playing time and a victim of a motor vehicle accident may not appreciate the nature of the injury.
A concussion is a diffuse injury without focal neurologic deficits such as pupillary dilation or limb weakness. The symptoms are usually subtle, such as dizziness and “seeing stars.” As per the Ontario Ministry of Tourism and Culture the most frequent symptoms are headaches, dizziness, nausea, imbalance, sleepiness, slurred speech, lack of coordination, sensitivity to light / noise, confusion, and forgetfulness. [5] The presence of just one of the latter symptoms is enough to diagnose a concussion; a person need not suffer multiple complaints.[6]
The diagnosis can be made only clinically because there is no proven biomarker based on imaging, blood tests or computerized neuropsychological screening tool. Conventional computed tomography (CT) and magnetic resonance imaging (MRI) scans almost always appear normal after concussions; even after repeated concussions. At this time there is no definitive objective test that can rule out a diagnosis of a concussion.[7]
Post-Concussion Management
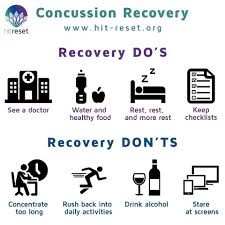
Removal from play, work or school, and rest are the most important aspects of initial management. Based on the consensus of experts, “rest” now includes rest from both physical and cognitive activities. This also includes the removal of certain stimuli such as watching television. No known treatment other than rest has proven to be successful for early management. If exercise is introduced too soon, it may bring on new symptoms and worsen old ones. A return to school, sports, or work should be on a graduated basis for physical and cognitive activities. [8]
The Minor Injury Guideline and Concussions
The law has recognized that a medical diagnosis of a concussion takes a claimant outside of the Minor Injury Guideline (“MIG”). As set-out by the adjudicator in N.K. v. Unica Insurance (2017) “concussion, post-concussion syndrome and related sequelae are not governed by the MIG”. The Adjudicator found that “the MIG relates only to minor injuries as defined by section 3(1) of the Schedule and this does not include brain injuries”.
In support of his case, the claimant relied upon medical evidence from his family doctor, an otolaryngologist, and a neurologist. The insurer relied on a neurologist to rebut the presumption that the applicant did in fact suffer any identifiable objective neurological deficits. Among other things the Adjudicator found as follows:
“mild injuries to the brain may not be observable in routine neurological exams, and sometimes the blow can result in microscopic damage to brain cells without obvious structural damage visible on a CT scan. I find that this effectively means that [the insurer neurological examination ] Dr. Baskind’s report (and the imaging results he references) is inconclusive with respect to concussion or post-concussion diagnoses.” [9]
In K.B. v. Echelon (2018), the dispute centred on whether the claimant had in fact suffered a concussion based on competing medical reports. The claimant relied upon a physiatrist who had an expertise in treating brain injuries who diagnosed a concussion four years post loss and the insurer retained a neurologist who found that there was no evidence to support such a conclusion. The claimant physiatrist found that the nature of the impairment to be “a concussion with post-concussive symptoms and this affects his ability to concentrate and attend to tasks and affects his mood, ability and as well he has generalized fatigue.” The insurer neurologist on the other hand found that there was no clear signs of ongoing post-concussion syndrome.[10]
The adjudicator accepted that the claimant suffered a concussion and that this by law took him outside of the MIG. He found that the IE neurologist “was looking for a clear sign of post-concussive syndrome. I do not require such a high bar”. The Adjudicator accepted that the diagnosis of a concussion is challenging and is not necessarily based on objective medical evidence.
However, claimants are being held to a stringent medical standard to prove the existence of a concussion. In DKD v. Aviva Insurance Canada (2018) [11] the claimant relied on a chiropractor who diagnosed the claimant with suffering from a concussion while as the insurer relied on medical reports from a neurologist and physician that concluded otherwise. The Adjudicator found that “a concussion diagnosis is outside of the scope of practice for a chiropractor” and accordingly rejected this finding. As such any conclusions reached by a non-medical doctor regarding the existence of a concussion and / or post concussion like symptoms will likely not be the deciding factor to a case. The Adjudicator found in favor of the insurer and the claimant was not taken outside of the MIG.

The Courts’ Treatment Of Concussions
In the recent decision of Abdulhussein v. Barbeau (2019), [12] the defendant brought a motion after the conclusion of trial to assert that the Plaintiff had not suffered an injury that crossed the threshold. In summarizing the medical evidence, the Judge was influenced by the fact that the claimant has been diagnosed with a post-concussive syndrome and suffered from a mild traumatic brain injury. The judge found that the claimant was cognitively impaired due to the head injury, chronic pain and depression all of which were all caused by the June 2, 2015 accident. The existence of the concussion and the ongoing impact on the claimant’s cognitive ability was an important factor that resulted in the defendant’s threshold motion to be dismissed.
In Doxtater v. Farrish, (2014),[13] the court accepted the evidence from an expert physiatrist with a specialty in treating brain injuries that there are rarely classic neurological signs associated with a mild brain injury. This explained why such an injury would not register on the various cognitive tests. The Court accepted the opinion of the physiatrist that “head trauma is not required for an acquired brain injury to occur”. Such an injury can be caused by the “whipping motion of the head during a collision”. When a brain injury is mild it will often not appear on an MRI, nor will it register on the Glasgow Coma Scale Test. The Court found that:
“Indeed, the myofascial soft tissue injuries that Ms. Doxtater exhibited in her neck, right shoulder, and right upper chest, as well as bruising she exhibited on her knees, support the conclusion that significant rotational forces were exerted on her head during the collision, which more likely than not led to an acquired brain injury.”
The Judge rejected the opinion of an expert defence neurologist who testified that a brain injury requires trauma to the head and will be revealed by objective findings either on an MRI or by the appearance of small lesions on the brain. The Judge disagreed with the neurologist’s opinion that the diagnosis of a brain injury is only within the purview of a neurologist as opposed to a physiatrist. The Judge accepted that the Plaintiff has suffered a concussion from this accident and ongoing post-concussive symptoms.
Conclusion
It is challenging to determine to what extent a claimant has suffered from consequences of a whiplash related injury or whether a mild brain injury such as a concussion has been sustained. The symptoms may appear to be similar such as headaches, dizziness, and problems with concentration. An individual need not suffer more then one symptom in order to have sustained a concussion.
In law, the decisions of Doxtater v. Farrish and N.K. v. Unica Insurance support the proposition that there is no reliable objective diagnostic test that will conclusively diagnose a concussion. Indeed, it is now recognized that an individual need not sustain a blow to the head to account for a mild brain injury; and that in only 5% of reported cases did an individual suffer an actual loss of consciousness. Despite the plethora of medical advances, the test to determine whether an individual has sustained a concussion is still based on the clinical impression of a doctor.
It is still the claimant’s obligation to prove his/ her case; including the diagnosis of a concussion. In DKD v. Aviva Insurance Canada the Adjudicator found that a chiropractor does not have the credentials to diagnose a concussion and the claimant was therefore unable to prove that his injuries took him outside of the MIG. Lawyers and adjusters should be cognizant that an opinion of a medial doctor is required to diagnose a concussion and not a chiropractor, physiotherapist and other non-medical treatment providers.
At the same time, it should also be recognized that the diagnosis of this condition is not solely within the purview of a neurologist. In K.B. v. Echelon and Fowler opinions rendered by a physiatrist with experience in treating brain injured patients was accepted over that a neurologist. Indeed, a treating family doctor or emergency doctor at a hospital will likely be the first medical practitioners to see a claimant shortly after an accident and their opinions will likely very influential.
While as most post-concussive symptoms resolve within three months, that is certainly not always the case. After an individual has suffered a concussion he/she becomes more susceptible to repeat injury and a protracted period of recovery. The law has recognized that the diagnosis of a concussion takes a claimant outside of the minor injury guideline and modern medicine tells us the best form of initial recovery is rest. As per the medical literature, a return to physical activities and / or substantive cognitive stimulation may not only impede a person’s level of recovery, but may also cause further substantive injury.
On the accident benefits side, the diagnosis of a concussion would often entitle a claimant at the outset to specific medical treatment to address this form of injury and in many cases support an entitlement to income replacement benefits / non-earner benefits. In circumstances where post-concussion symptoms are ongoing this may support an ongoing entitlement to income loss and evidence to support a threshold type claim.
In short, mild traumatic brain
injury cases are difficult to address both from a medical and legal
standpoint. It is challenging to
determine whether an individual who is suffering from symptoms of soft tissue
based chronic pain may also have suffered a concussion. There are likely many claimants who have
suffered undiagnosed concussions who continue to struggle as they have not
received the proper treatment. At the
same time, adjusters are being tasked to determine to what extent a legitimate
concussion has been sustained and whether there are any long-lasting
repercussions from same. These are not
easy issues to address from both the adjuster and claimant standpoint. While as there are many challenges inherent
to the unknowns of concussions, knowledge of the medicine and the law will make
us better at our jobs. We will
understand the intricacies of concussions in relation to insurance law and make
better informed decisions to advance our cases.

Cary N. Schneider is a co-founder of Schneider Law Firm who specializes in civil litigation including personal injury litigation, real estate litigation, cyber / privacy breaches, and commercial litigation. After working on behalf of insurance companies for 19 years he now uses that inside knowledge to the benefit of his clients. He is proud to have received referrals from insurance defence lawyers and represents adjusters in their personal injury matters. He has been rated by Best Lawyers Canada, Lexpert Rated Lawyer, and Martindale-Hubble for his litigation skills. If you or a loved one has suffered a personal injury contact Cary to let him assist them in their time of need. Email cschneider@schneiderlawfirm.ca or call at 416-849-6633 x 201. www.schneiderlawfirm.ca.
[1] Post Concussion Syndrome Mayo Clinic, 2017
[2] Concussions And Their Consequences: Current Diagnosis, Management And Prevention, Dr. Charles Tator, The Canadian Medical Association Journal
[3]Ibid 2
[4] Ibid 2
[5] Ontario Ministry of Tourism, Culture and Sport
[6] Ibid 2
[7] Ibid 2
[8] Ibid 2
[9] N.K. v. Unica Insurance (2017) 17-001473 LAT
[10] K.B. v. Echelon (2018) 18-000655 LAT
[11] DKD v. Aviva Insurance Canada (2018) 17-009018 LAT
[12] Abdulhussein v. Barbeau (2019) ONSC 966
[13] Doxtater v. Farrish, (2014), ONSC 4224

Leave a Comment